
Ramsey MHK accuses government of prioritising cost-cutting over patient safety and claims healthcare plans push public towards private sector
Ramsey MHK Lawrie Hooper has raised serious concerns over the Mandate to Manx Care and the accompanying 2025–26 Operating Plan, describing them as "inadequate" and warning that they could lead to an "unacceptable reduction in services" for the Manx public.
In a motion tabled before Tynwald, Mr Hooper called for the Department of Health and Social Care to produce revised documents which, he said, should avoid significant curtailments to frontline services, fully implement recommendations from bodies such as the Care Quality Commission and Ofsted, and avoid replacing NHS provision with private healthcare alternatives.
He also proposed that any updated Mandate and Operating Plan be brought to Tynwald for debate and approval in July 2025.
Acknowledging the government’s automatic voting majority due to the number of ministers and a current absence of two MHKs, Mr Hooper said he did not expect the motion to succeed. However, he urged fellow members to vote with their conscience, warning that they would be held accountable by constituents at the next general election.
Describing the Mandate as a statutory document which underpins healthcare delivery, Mr Hooper criticised the health minister’s suggestion that it is “open to interpretation”. He argued that this position risks undermining accountability and could allow for the document to be altered ‘on the fly’, presenting what he called ‘huge risks’.
He pointed to a number of perceived inconsistencies in the Mandate, particularly in relation to funding.
Mr Hooper noted that while the Pink Book lists Manx Care’s budget as nearly £357 million, the Mandate refers to £361.8 million – a figure which he said appears to include contingency funding defined by Treasury.
He questioned which of either the Mandate or the minister’s statements were incorrect and warned that the financial plan hinges on a £15 million cost improvement programme, while overspending is projected to be in the region of £20 million.
He suggested that the health service is being asked to save as much as eight percent of its total annual budget. If members voted in favour and deemed that 'reasonable', he said he would bring forward further motions calling for all government departments to deliver similar savings.
He also questioned the reliability of the assumptions underpinning the Mandate, claiming Manx Care itself had identified unbudgeted and unforeseen pressures.
To illustrate his concerns, he said he ran the document through an artificial intelligence analysis tool, which summarised the risks as reduced access to acute care and increased reliance on private options.
Mr Hooper criticised the performance targets outlined in the Mandate, saying they appeared to measure “widgets, not outcomes”. He argued that many objectives would not improve quality of life and said some statistics were “meaningless” or unrealistic. He also highlighted apparent contradictions between the DHSC and Manx Care, particularly over expectations for A&E waiting times and access to care.
Children’s services, respite care, and autism provision were singled out as areas of major concern. Mr Hooper said he was “incredulous” that support for some of the Island’s most vulnerable people appears to have been deprioritised due to budget constraints, which he labelled “completely disgraceful”.
He said the approach outlined in the Mandate reflects a view that “the budget is the budget”, which he questioned as a valid approach to running a government.
Describing the documents as a “huge assault on frontline services”, Mr Hooper said that despite the issues he raised, the Mandate and Operating Plan likely represents the “best case scenario” under current funding plans, and warned that the situation could deteriorate further if financial pressures worsen.
While acknowledging longstanding cultural and financial issues within the health system, he warned that attempting to implement rapid change without appropriate resourcing would lead to worse outcomes for patients.
Concluding his speech, Mr Hooper said the Mandate appeared to push the public towards private healthcare providers.
“I would much rather spend the money than spend the patient.
"You can get money back, but you can't get lives back."
Douglas East MHK Joney Faragher
Joney Faragher rose to second the motion, warning that the current direction of travel in healthcare planning would risk worsening health outcomes and further entrenching inequalities.
Ms Faragher expressed concern that proposed reductions in hospital capacity, particularly inpatient beds, would place unsustainable pressure on community health services. She criticises what she describes as an over-reliance on the voluntary and third sector to absorb this pressure, labelling it “unacceptable”.
Referencing previous efforts to reduce waiting lists, Ms Faragher said she feared the gains made through recent investment would be “undone” by the new Mandate and Operating Plan. She highlighted the deprioritisation of key preventative services, and raised alarm at the lack of reference to autism care and suicide prevention, warning that their absence would contribute to “increasing social issues”.
She argued that the Mandate contradicted the stated ambitions of the Island Plan, which commits to improving waiting times and enhancing health and wellbeing. “The actions outlined in the Mandate undermine those aims,” she said, questioning whether the Council of Ministers had fully considered its own policy commitments.
Echoing earlier concerns about the impact on equity, Ms Faragher warned that patients with limited financial means may be left behind.
“Those who can afford to pay will be able to get better, but those who can’t are forced to suffer,” she said.
She also criticised proposals to restrict off-Island referrals, which she describes as essential for some patients and “not a luxury”. She claims such decisions reflected a pattern of political short-termism that would lead to “worse outcomes and higher costs” in the long run.
Ms Faragher questioned the proposed £500,000 reduction in administrative costs, suggesting that it may lead to increased burdens on frontline clinical staff. She also pointed to what she called a “subtle but undeniable” shift towards private healthcare, noting the Mandate’s instruction to “explore increasing private options” on the basis that it would ‘enhance patient choice’.
Raising issues around governance, Ms Faragher referred to conversations between senior Manx Care officials and off-Island providers. She said there were serious concerns about whether providers were continuing with treatment plans in good faith, despite uncertainties around payment, and questioned if Manx Care leadership fully understood the implications of their actions.
She ended with a direct message to the government:
“This will be a burden we are passing onto future generations. Every member of the Council of Ministers should examine their own conscience and principles.”
Glenfaba and Peel MHK Kate Lord-Brennan
Kate Lord-Brennan acknowledged concerns raised by other members, but she also commended the Department of Health and Social Care for what she described as a willingness to confront difficult and long-standing issues.
‘It’s all very well handing out severe criticism, but credit should be given where it’s due for trying to tackle the problems’, she said.
Ms Lord-Brennan noted a ‘tighter grip’ and clear intent within the Department, and recognised the difficult compromises Manx Care faces in balancing competing needs and demands.
Ms Lord-Brennan sought to introduce an amendment to the motion that would give the Department of Health and Social Care responsibility for determining funding allocations to Hospice Isle of Man and third sector organisations delivering essential health and social care services. She proposed that the Manx Care budget be adjusted accordingly to reflect this.
Arguing that these vital community organisations should remain close to the political sphere in terms of funding oversight, she emphasised the particular importance of palliative care. “It’s a moral responsibility, and reflects how we as a society choose to treat people as they approach the end of their lives.”
Her remarks followed a recent appeal by Hospice Isle of Man, which requested Tynwald review its funding allocation after receiving £1.7 million - substantially less than the £2.3 million it had requested to maintain its current level of service.
Ms Lord-Brennan called for end-of-life care to be brought back under direct political oversight, stating that Hospice should be regarded as a core public care partner, deserving of “our care, attention and support”.
Onchan MHK Rob Callister
Rob Callister also added his voice to the debate, calling for a fundamental reset in the relationship between the Department of Health and Social Care and Manx Care, while urging Tynwald to support a period of stability and reform within the department.
Mr Callister expressed disappointment that a general debate on health reform had not taken place sooner, and said it was time for “honest and frank conversations” about the challenges the Isle of Man faces in building a sustainable healthcare system.
He argued that the partnership between the DHSC and Manx Care had not functioned as intended, and said the existing relationship “must be reset quickly.” He was clear in stating that Manx Care could not be solely held to account for ongoing issues, instead pointing to what he described as a “clear lack of leadership” at both political and senior executive levels within the DHSC over the past three years.
“The Department of Health and Social Care cannot help, support or even hold Manx Care to account for its own operational performance,” he said, “until it can sort out some of its own deep-rooted issues.”
Mr Callister called for the department to be reshaped, with a clearer focus on its priorities, strengthened leadership, and open communication with staff. He stressed that those working within the system must feel “informed, supported and listened to”, particularly in the face of potential structural or cultural changes. “This department has been seriously let down on all levels over the past four years,” he said, adding that he hoped for improvement through greater support from central government and Tynwald.
He said the Island must now grapple with the “very difficult conversation” of how to build a future-ready health service, and suggested that greater political oversight of Manx Care operations should now be seriously considered.
Mr Callister raised concern over the feasibility of fully integrating health and social care on the Island, suggesting that long waits for vital services had become “routine”, and public satisfaction remained low. Reflecting on the Mandate and Operating Plan, he stated he had “little or no confidence” in many of the assurances contained within.
He warned that the Mandate pointed to a “significant risk” of reduced outpatient and other clinical activities, and voiced concern about senior pay levels in the health sector.
Specifically, he questioned whether the Isle of Man was overpaying for senior managers and consultants, particularly at Noble’s Hospital. He called for a comprehensive review of all roles within Manx Care, to be benchmarked against equivalent NHS positions in England, Scotland, Ireland, and the Channel Islands, in the interests of fairness and value for money.
“This situation is wholly unacceptable,” he concluded, “especially considering the significant investment made over the past four years.”
In closing, Mr Callister quoted the UK Health Secretary Wes Streeting, saying:
“If we get this right, we can look back on our time with pride and say that we were the generation that took the NHS from the worst crises in its history, got it back on its feet and made it fit for the future.”
Attorney General Walter Wannenburgh
In a rare intervention, the Isle of Man’s Attorney General, Walter Wannenburgh, provided legal clarification on the constitutional boundaries surrounding the Manx Care Mandate and Operating Plan.
Mr Wannenburgh reminded members that under the Manx Care Act, the power to revise the Mandate lies solely with the Department of Health and Social Care, and any amendment would also require the agreement of Manx Care, and could only be considered under exceptional circumstances.
He stressed that there is no statutory requirement for Tynwald to approve the Mandate or the Operating Plan, stating these provisions were deliberately established when Manx Care was created.
Mr Wannenburgh further clarified that the DHSC holds the legal responsibility to produce the Mandate, while the legislation does not impose any duty on the Department to formulate the Operating Plan. That responsibility lies with Manx Care itself.
While acknowledging that the DHSC had fulfilled its legal obligation by producing a Mandate, the Attorney-General emphasised that Tynwald does not have the authority to override, amend, or invalidate the document through a parliamentary motion.
“Tynwald cannot overrule the Mandate without introducing new legislation to override or suspend, displace, or replace existing provision”.
As the law stands, any motion passed in Tynwald expressing an opinion about the Mandate or Operating Plan would have no legal effect. He told Tynwald the existing provision makes ‘no room’ for opinion by Tynwald to have any effect or consequence.
Mr Wannenburgh concluded that, as a matter of law, only the DHSC can revise the Mandate, and only Manx Care can amend the Operating Plan. Therefore, he said, the motion under debate would have “no legal basis nor effect”.
Arbory, Castletown and Malew MHK Tim Glover
Tim Glover added to the debate by calling for a constructive and solution-focused approach to concerns raised in the Mandate and Operating Plan, while emphasising the importance of patient outcomes over organisational efficiency.
Mr Glover began by acknowledging the efforts of the Health and Social Care Minister, stating that he felt for her position and recognised the limitations within which she was working. However, he cautioned against descending into a “tit for tat” exchange and instead urged members to focus on the specific issues within the documents under discussion.
Among his key concerns was the absence of references to autism support and suicide prevention strategies in the Mandate. “It is disturbing that we have no reference to these areas,” he said, warning that gaps in such vital areas of care could result in long-term social consequences.
He raised concerns that some patients were already turning to private healthcare due to delays in accessing services, shouldering the financial burden themselves. “It’s a very real situation,” he said, highlighting the growing divide between those who can afford private treatment and those who cannot.
Mr Glover drew a distinction between efficiency and effectiveness, stating that while the system appeared focused on process and structure, it risked losing sight of its core purpose: delivering better outcomes for patients. “We need to put the patient first, rather than structures,” he said, renewing his call for a full audit of Manx Care to properly assess its financial management and performance.
He welcomed the apparent resolution of uncertainty around the future of the Island’s air ambulance service, which had been threatened by funding issues, but expressed reservations about its long-term security. “It resembles a plaster on a wound, rather than a plaster on a cut,” he said, suggesting that more sustainable solutions were needed.
Mr Glover was also critical of the Mandate’s clarity and direction, stating that it lacked the decisiveness expected of a legal document. Reflecting on previous government investment aimed at reducing waiting lists, he said the promise that they would not grow again now appeared to be “just warm words”.
He also raised issues with Manx Care’s complaints handling process, claiming that the organisation often went into “defensive mode” when formal complaints were raised. “Most people aren’t looking for financial compensation,” he said, “they just want answers.”
Concluding his remarks, Mr Glover posed a question to fellow members:
“What price do we put on safety? Efficiency versus effectiveness – that is my message to you today.”
Health and Social Care Minister Claire Christian
Claire Christian delivered a robust defence of the Mandate to Manx Care and the accompanying Operating Plan, rejecting accusations that the documents represent a deliberate scaling back of patient services or a shift towards privatisation.
Responding to criticism from several members, including Ramsey MHK Lawrie Hooper, Minister Christian said she strongly objected to “personal interpretations” of the documents, particularly where she felt her own comments had been taken out of context.
While acknowledging that communication could be clearer, she stood by the work of the Department of Health and Social Care and confirmed she would be voting against the motion.
Since assuming her ministerial role, she said, her priority has been ensuring health services are delivered within an agreed and sustainable budget. She outlined the broader challenges facing the Island’s health system, including an ageing population and rising expectations driven by advances in medicine and science. “We’ve extended life expectancy, but more people are living with complex conditions that require attention,” she said.
Minister Christian emphasised that the modernisation of services was not driven by cost-saving motives, but by a desire to do what is right for the Island and its population. “This is not about money,” she said. “It’s about creating a system that meets today’s needs and tomorrow’s challenges.”
She reiterated a strong commitment to the founding principles of the NHS and refuted claims that the Mandate seeks to reduce patient services.
She clarified that the Department’s aim to avoid hospital-based care where appropriate is rooted in clinical best practice - ensuring patients are treated in the most suitable setting, rather than funnelling all demand into acute services.
On the issue of off-Island appointments, Minister Christian stated clearly that such referrals should only be used when suitable care cannot be delivered on-Island. She also addressed concerns raised about private healthcare options, stating that there was no push to replace NHS services with private provision. Instead, she explained that signposting private care is about offering choice to those who seek it, and that private practice has the potential to generate income and attract clinicians to relocate to the Isle of Man.
Responding directly to Douglas East MHK Joney Faragher’s concerns about a lack of community services, she stated that these claims were incorrect and that services would be in place to support patients outside of hospital settings.
Concluding her speech, Minister Christian reaffirmed her commitment to openness and transparency, and expressed gratitude to the politicians, civil servants, and health professionals involved in developing the Mandate and Operating Plan.
Legislative Council Member Paul Craine
Paul Craine also contributed to the Tynwald debate, countering remarks that the Department of Health and Social Care is deprioritising patient care, while calling for greater realism about the challenges facing the health service.
Mr Craine described allegations that the Department is shifting its focus away from patients as “absolutely not true”.
He made remarks with references to UK mortality statistics, and noted that the percentage likelihood of dying at pre-retirement age remains relatively low, but that the demographic shift itself poses significant challenges.
He pointed out that a growing proportion of the population is entering older age groups, which he said inevitably leads to more people living with complex and long-term conditions.
“The reality of an ageing population is that the burden on health services will become increasingly difficult to manage. It will be an uphill battle all the way.”
Mr Craine raised the possibility that in the future, individuals who have the means to do so may be encouraged to contribute towards their own care. Although he wasn’t advocating for a shift away from publicly funded healthcare, he acknowledged that the pressures may prompt broader conversations about the role of private contributions in the future.
He sought to place the state of the Isle of Man’s health service in a wider context, suggesting that public perceptions may not always reflect the reality on the ground. Drawing comparisons to images of patients waiting in hospital corridors in the UK, Mr Craine argued that the Island’s health service, while facing real pressures, remains in a relatively better condition.
He concluded by stressing that the rising cost of healthcare is a global issue and that the challenge of keeping pace with those costs - particularly in light of an ageing population - is one shared by many nations.
Cabinet Office Minister David Ashford
David Ashford offered a brief contribution to the debate, using his remarks to highlight both early signs of progress and the need to view the Island’s healthcare challenges within a broader international context.
Minister Ashford revealed that during his lunch break, he had experimented with artificial intelligence by training a model using multiple previous Manx Care mandates alongside the Sir Jonathan Michael Report, a key review of the Island’s health and social care system.
He said that, based on this exercise, the AI had identified what he described as “green shoots” of progress in the Island’s healthcare planning and delivery. While acknowledging ongoing concerns, Mr Ashford stressed that the pressures being experienced are not unique to the Isle of Man, but are part of a wider global struggle to deliver effective and sustainable healthcare.
Douglas North MHK John Wannenburgh
John Wannenburgh delivered a forthright critique of the health Mandate and funding arrangements, warning that current decisions risk shifting the burden onto future administrations and calling on government to meet the true financial needs of the health service.
Mr Wannenburgh said that, regardless of how it is ‘spun’, there is insufficient funding within the health service. He described the Mandate as a direct response to the limitations imposed by the health budget, arguing that meeting those constraints has forced Manx Care to apply strain to certain areas of service.
He pointed to increased pay for doctors as a source of additional pressure on the budget, suggesting that the disparity was already placing strain beyond what had been allocated.
Mr Wannenburgh claims he regularly sees comments calling for the removal of Manx Care and for the reintegration of healthcare back under the Department of Health and Social Care. However, he pushed back on this idea, claiming that Manx Care has become a challenging and “toxic environment” to work within, but that reverting to departmental control would repeat past mistakes. “History shows us what happens when we place tasks in the hands of civil servants, yet this is exactly the proposal by some.”
He also questioned the motives behind recent funding boosts given to Manx Care, suggesting they were prompted more by ‘political fear’ than long-term strategic planning.
Mr Wannenburgh said much of the increased funding set out in the Pink Book was being consumed by staff pay uplifts and rising drug costs, rather than resulting in improved service provision, arguing more money is being spent, just to ‘stand still’.
He warned that the current approach risks deferring consequences rather than addressing them, accusing the government of using the Mandate to “push the repercussions into the next administration” - a move he called “unacceptable”.
Urging ministers to match the funding required to meet the Island’s health needs, Mr Wannenburgh concluded by quoting the late Apple co-founder Steve Jobs:
“Leadership is hard. If you want to make everyone happy, don't be a leader, sell ice cream.”
Chief Minister Alfred Cannan
Alfred Cannan approached the debate by offering a defence of the Mandate and Operating Plan, while acknowledging the scale of the challenges ahead and the imperfections in the current documents.
Mr Cannan began by paying tribute to the minister for health and social care, officials at Manx Care, and senior civil servants involved in preparing the Mandate and ensuring that the Operating Plan was ready for release alongside it.
He noted that, structurally, Tynwald is limited in what influence it can exert over these processes, given the statutory responsibilities set out in law.
While acknowledging that the Mandate would be difficult to deliver, he warned that the Isle of Man now stood at a “crossroads”.
“This government has pumped more money into the health service than any other,” he said, pointing to an investment exceeding £100 million, including significant funding to reduce waiting lists.
However, he warned that this debate was less about specific policies and more about broader principles.
“We cannot go on with a shrug of the shoulders,” he said, warning that healthcare funding would otherwise grow to ‘dominate’ public expenditure, leaving little room for other priorities - or leading to taxation levels that could, “deteriorate our economy before our eyes”.
He posed a key question to members and the wider public: whether people are prepared to pay more in taxation for services they feel are not currently meeting expectations.
While acknowledging that Manx Care remains a relatively new organisation, Mr Cannan expressed confidence in its potential and said it has “plenty of scope to sort itself out”. He accepted that many people believe service standards are below acceptable levels and recognised the additional pressures caused by an ageing population and the wider inflationary environment.
He also noted ongoing concerns about internal dynamics within the health service. “There has been far too much evidence of in-fighting,” he said, stressing that the health service must “get tough with itself” and improve internal cohesion.
He argued that aligning the Mandate to the Operating Plan was long overdue, and while the documents are not perfect, he maintained they represent necessary and pragmatic steps forward. “It’s absolutely right that politicians express concerns,” he said, “but we are taking the steps needed to sort out the issues with the money available.”
Mr Cannan concluded by saying that printed documents alone are not sufficient to deliver results. Instead, he called for a cultural shift within the health service - empowering those working under budget constraints to innovate and deliver services more productively.
He ended with a message of cautious optimism:
“The Island is facing increasing demand for services, but this Mandate and Operating Plan are crucial first steps. We are not alone in these challenges, but it is important that we face up to them.”
Member of the Legislative Council Gary Clueit
Gary Clueit warns that while concerns about healthcare delivery are valid, the motion under consideration would not resolve them - and may instead make the situation worse.
Mr Clueit asked rhetorically, “How much exactly should be spent on health and social care? Well, how long is a piece of string?” He acknowledged that public finances are not limitless and that difficult decisions must be made - decisions which “will always displease some.”
He reflected on the scale of structural reform underway, stating that no major organisational change occurs without pain. In his view, the best-case timeline for meaningful transformation is five years - even under ideal conditions, let alone in the shadow of a pandemic that disrupted the early years of Manx Care’s existence.
Drawing on his business background, Mr Clueit suggested that any organisation undergoing financial strain would ordinarily seek to reduce overheads before considering cuts to its workforce or core services. While he expressed concerns about the direction of the health service, he made clear that he does not believe the motion under debate offers a viable solution, and could potentially deepen uncertainty.
Mr Clueit questions some of the priorities set out in the Manx Care Operating Plan. He believes waiting lists remain the most pressing issue for residents, yet tackling these delays is complicated by what he described as years of “mal and non-compliance” with Care Quality Commission standards. Addressing this legacy will take considerable time, he warns.
He acknowledged the stark reality outlined by Manx Care - that delivering the Mandate in its current form may require service reductions. In his view, it might be more appropriate for government to formally scale back the scope of mandated services rather than risk overpromising and underdelivering.
Discussing the prospect of privatisation, Mr Clueit was clear in his opposition to its provision within NHS facilities. He argued that individuals with greater means should contribute more, and appeared to show support to the idea of introducing a healthcare levy, provided it does not place additional burdens on lower-income households.
Douglas Central MHK Chris Thomas
Chris Thomas used his contribution to call for a more honest and reflective public dialogue on what the Isle of Man’s healthcare system can realistically achieve, and urged structural reform to give elected members greater influence over Manx Care's direction.
Referring to a question raised previously by a Tynwald committee, Mr Thomas asked: “To what extent is the Island willing to accept the reality of what is possible to do within its healthcare system?” He said this encapsulates the heart of the current debate, one that revolves not only around policy detail, but around the fundamental values and limitations of public health provision.
He acknowledged that there are, and should be, differing views on how to navigate the current challenges, but said the debate itself represents a vital opportunity to capture the essence of what healthcare means to the Island's population.
Mr Thomas highlighted that while Manx Care has come under sustained criticism during the sitting, the organisation itself does not have a voice in Tynwald.
He said there are indeed achievements that Manx Care could point to, and this should be recognised in a balanced assessment. As part of his efforts to address this, Mr Thomas noted that he had advocated for political representation on the Manx Care board.
He also made a procedural point, suggesting it would be possible for Tynwald to amend the Manx Care Act in a single day, if there was the political will to do so. He argued this would allow Tynwald to play a more active role in shaping healthcare policy, including the Mandate and Operating Plan.
Looking back, Mr Thomas said that both he and Ramsey MHK Lawrie Hooper had warned during the creation of the Manx Care Act about clauses which, he believes, are now contributing to the issues being experienced today.
Legislative Council Member Dawn Kinnish
Dawn Kinnish warns that the failure to provide adequate support for individuals with learning disabilities and communication needs could result in greater social and financial costs in the future.
“If there’s a risk of non-delivery of services, you risk a much greater cost later on.”
Ms Kinnish expressed alarm that those with learning disabilities were largely invisible within the Mandate. She argued that existing data already highlights critical gaps and appears to have been overlooked.
One of her key concerns was the lack of advocacy provision for people with learning disabilities. She explained that advocacy plays a vital role in helping individuals understand their care processes and express their thoughts, beliefs and concerns - particularly where they may struggle to do so independently. “In the UK, it is a statutory duty,” she noted. “The Isle of Man used to provide it, but this service ended.” She called for its reinstatement, saying its absence leaves vulnerable individuals without a voice in decisions affecting their lives.
Ms Kinnish also raised concerns about respite care, stating that current options are “non-existent” due to insufficient capacity. She described a scenario where families in crisis are left with no choice but to hand their child over to the state - an outcome she said could have been avoided if adequate respite care were available.
Turning to speech and language therapy, Ms Kinnish claimed that services for those with speech and language needs had been “completely overlooked” in the Mandate.
She presented figures from December 2024, stating that while there were 2.6 full-time equivalent speech and language therapists working in mainstream schools - each with an average caseload of 53 - there was only a 0.5 full-time equivalent therapist assigned to specialist provisions, supporting approximately 110 individuals.
“If you have a disability, you will not get the same access to the same level of support as someone without a disability. This is clear discrimination.”
Ms Kinnish urged the Department of Health and Social Care to address these disparities as a matter of urgency.
Onchan MHK Julie Edge
Onchan MHK Julie Edge delivered a deeply personal speech, criticising what she described as years of failure and mismanagement under the Manx Care model. She reiterated concerns she has raised in previous debates, saying they remain just as relevant today as when Manx Care was first established.
Ms Edge characterised the health body’s trajectory as one marked by a "catalogue of failures", and questioned the continued reliance on the Sir Jonathan Michael Report, which she described as outdated. “He made recommendations, not legally binding requirements.”
Citing the reduction in operational hospital beds - from 361 when Noble’s Hospital opened, to 183 today - Ms Edge questioned the logic behind this shift. “Common sense would tell you it’s not a good idea, and then we wonder why waiting times have increased.”
She described the decision to make Manx Care a fully arm’s-length body as ‘the biggest error’, arguing that it created an organisation that is difficult to scrutinise and insufficiently accountable.
Since its inception, Manx Care has had access to increasing budgets with “very little scrutiny”, she said. She likened the situation to a failing project being continuously funded without any meaningful oversight, saying: “If I went back to my bank manager because my project had run out of funding, I would have to hand over a detailed breakdown of every pound that was spent. Yet Manx Care has never been asked to do that.”
“Manx Care has created an empire that is haemorrhaging money year on year.”
Ms Edge said she believes public confidence has collapsed, and claimed “the whole of the Island is crying out for Manx Care to be abolished.” To that end, she tabled an amendment calling for the Tynwald Auditor General to carry out a full value-for-money inspection into all of Manx Care’s functions. She also called for the creation of a ‘Professional Executive Committee’ at Noble’s Hospital, as proposed by the Isle of Man Medical Society, to ensure clinical oversight and restore professional governance.
Rejecting arguments that rising doctors’ pay is at the root of financial pressure, she warned colleagues not to be “gaslighted” and said the problem lies in a managerial structure that the public sees as “top-heavy” and unable to deliver safe, effective services.
Ms Edge raised serious concerns about compliance with European Court of Human Rights standards, suggesting that prolonged delays in care are putting patients at risk of harm, particularly in primary care where backlogs are feeding into overburdened secondary services. She cited dental care as one example: “You now don’t get a six-month check-up, you get a 12-month one, but the waiting list is still increasing.”
She said claims that cancelling services saves money are deeply flawed. “The costs come back in future years. That is not financial responsibility - it’s financial irresponsibility.”
In an emotional moment during her speech, Ms Edge shared a personal experience, describing receiving a 'dangerous letter' that removed her from an endoscopy waiting list. When she contacted the hospital to ask who had made the decision, she was told no one could say. “Even clinicians were shocked when they conducted the treatment."
“Is this negligence? This needs auditing. It is not a patient-centred approach. I have real, serious concerns and the public deserves answers.”
Arbory, Castletown and Malew MHK Jason Moorhouse
Jason Moorhouse gave his backing to Julie Edge’s proposed amendment calling for the Tynwald Auditor General to carry out a full value-for-money audit into the functions of Manx Care.
He also raised a more provocative idea, suggesting that the government consider commissioning a private provider to conduct a full-scale review to determine the actual operational cost of running Manx Care, given as much as £1 million per day is allocated to its operating.
The suggestion appeared to cause visible confusion among some members in the chamber, with questions arising as to whether Mr Moorhouse was advocating for the entire health service to be outsourced to a private company. Responding to those concerns, he clarified that the idea was merely a thought experiment – ‘an extreme’, as he described it - and not a formal proposal.
He emphasised that in such a model, the Department of Health and Social Care would retain full oversight and control, and the role of any private operator would be limited to operational delivery, rather than policy or governance.
Legislative Council Member Peter Reid
Peter Reid, a political member of the Department of Health and Social Care, began by expressing disappointment that such a significant discussion had not taken place during the previous sitting, but ultimately voicing support for the current approach outlined in the Mandate.
Responding to criticism that the Mandate merely "kicks the can down the road", Mr Reid said he disagreed with that characterisation.
In his view, the document represents a fundamental shift in the Island’s healthcare strategy - one that demands a longer-term view.
Reflecting on his own background in major business, Mr Reid emphasised the importance of focusing on value in care and service delivery, rather than equating improvement solely with increased expenditure.
“Care and service in terms of value is what we should all be focused on,” he said, cautioning against what he described as the instinctive “more money” solution to complex problems.
He stated that he would be voting against the motion - not only because of the legal clarification offered by the Attorney General, which indicated that the motion has no binding effect - but also because he does not believe that further funding alone will solve the systemic challenges within Manx Care and the health system more broadly.
Legislative Council Member Diane Kelsey
Diane Kelsey, who also serves as a member of the Department of Health and Social Care, used her contribution to reinforce a number of key principles underpinning the Island’s health service reforms, while acknowledging the complexity and challenges ahead.
She began by affirming her belief that health services must always be based on clinical need, rather than a patient’s ability to pay.
Mrs Kelsey expressed her agreement with fellow MLC Peter Reid, particularly his argument that healthcare reform must be driven by long-term thinking and value, rather than a reflexive call for additional funding. She also pointed to the Operating Plan’s ‘clear prioritisation of primary care’, and said she was confident that the health service recognises the issues in this area and is actively working to address them.
Responding to earlier comments by MLC Dawn Kinnish regarding service gaps - particularly for individuals with learning disabilities - Mrs Kelsey acknowledged that while some of those concerns may already be addressed within current planning, “it might not be enough.” She agreed that understanding what is going wrong, and why, is essential to making improvements.
She also highlighted inefficiencies in the hospital system’s digital infrastructure, stating that staff must navigate as many as eight separate authentication systems simply to log in. “That cannot be the right thing to do,” she said, arguing this is a barrier to efficiency that undermines the effectiveness of care delivery.
While acknowledging the inherent difficulties of large-scale change, Mrs Kelsey said she believes there is a clear process in place and that scrutiny mechanisms are available. She indicated that future business cases will address many of the known risks, and emphasised that the Island has a roadmap for transformation already outlined in its strategic planning.
Lastly, she reflected on the Sir Jonathan Michael Report, which has formed the foundation of recent health reforms. She believes its recommendations remain broadly relevant, but raised the question of whether they still represent the right direction for the Island today: “Is it still the right path to take?” she asked.
Legislative Council Member Tanya August-Philips
Tanya August-Philips appealed for collective leadership and long-term vision, framing the Island’s NHS provision as a core pillar of quality of life and social values.
“The Island’s NHS provision is the cornerstone to the quality of life. How we steward it speaks to what sort of society we want to live in - now and in the future.”
Mrs August-Philips emphasised that while the system has not always met expectations, past efforts should not be dismissed. “We should accept that we haven’t always got it right. But every effort is not wasted.”
Reflecting on the creation of Manx Care and the implementation of recommendations from the Sir Jonathan Michael Report, she acknowledged the significant structural shift in separating operational healthcare from political oversight. While the desire for rapid, tangible improvements was understandable, she said transforming the system is a slow and complex process. “Turning the ship around is no easy feat,” she noted, while also recognising that there have been interventions that have helped reduce waiting lists.
“At times the road is bumpy, but we’re not at the destination yet.”
Mrs August-Philips highlighted that while members may approach healthcare reform from different perspectives, they remain united in their ambition to deliver the best outcomes for the people of the Isle of Man. She stressed that the public is looking to Tynwald and government for leadership - particularly in facing difficult decisions head-on.
She acknowledged that there is limited time remaining in the current administration but insisted that important work can still be done. However, she suggested that the political focus on the Mandate and Operating Plan may have come at the expense of addressing core issues - namely, public dissatisfaction with the service relative to the level of taxation and expectation.
“Residents feel they are not getting what they pay for.”
Describing her own comments as “a small pea in a large pie,” Mrs August-Philips admitted that much work remains - particularly in light of findings from the Care Quality Commission and Ofsted, which have brought systemic weaknesses to light.
Despite the often emotive nature of the debate, she concluded on an optimistic note: “This debate has given me hope for the future.”
Legislative Council Member Kirstie Morphet
Kirstie Morphet, told Tynwald she had not originally planned to speak, given her recent employment within Manx Care.
However, she expressed her inability to support the motion brought forward by Ramsey MHK Lawrie Hooper, citing the clear legal advice provided by the Attorney General regarding its lack of enforceability.
Mrs Morphet explained she felt compelled to speak after listening to the wide range of views expressed. One of her key concerns was the ongoing lack of progress in addressing the funding of adult social care, an issue she said continues to be overlooked.
“There has been no movement on how to fund adult social care,” she said, warning that without properly resourced and accessible preventative measures, more individuals would end up requiring hospital treatment - putting further strain on acute services.
Responding to wider commentary in the debate, she firmly rejected any suggestion that frontline staff are not working to full capacity.
Drawing on her own experience, Mrs Morphet said, “My experience is the opposite,” and extended her thanks to health and social care workers, many of whom she noted are among the lowest paid, yet carry out some of the most challenging roles on the Island.
Environment, Food and Agriculture Minister Clare Barber
Clare Barber commending the Department of Health and Social Care and Manx Care for what she described as a “robust” and committed approach to patient care, while identifying communication as an area in need of improvement.
She referred to a recent media report which incorrectly suggested that a senior figure at the Great North Air Ambulance had stepped down due to uncertainty over its operations and partnership with the Isle of Man. Minister Barber clarified that the report had been inaccurate and was promptly corrected once flagged.
Turning to the broader political discussion, she expressed concern at calls for increased political control over areas she believes must remain in the hands of clinicians.
“I have great concern that there are calls for increased power for politicians to have control over areas that have to be kept within the clinicians."
Addressing ongoing concerns about the perceived privatisation of health services, Minister Barber sought to provide clarity. She noted that many people already pay for elements of their healthcare - such as prescriptions, glasses, and dental care - and that private sector support to reduce waiting lists has long existed without being labelled as privatisation. “I’ve never heard these referred to as privatisation of the NHS,” she said.
She urged members to be mindful of the language they use when discussing the future of the health service. “We have a responsibility to be careful about what we say,” she warned, adding that the public debate must not undermine confidence in the system. She also called on the media to act responsibly by prioritising facts over sensationalism.
Concluding her remarks, Minister Barber praised the dedication of health workers and clinicians, saying they need political support, not division.
“They need politicians to build them up and work with them to make the health service the best it can possibly be. That can only be achieved if we all work together.”
Douglas Central MHK Ann Corlett
Ann Corlett drew on her experience as a former member of the Department of Health and Social Care in the previous administration.
Mrs Corlett recalled that during her time in the Department, officials were routinely “firefighting” to maintain acute services, often at the expense of social care. The pressure to control a spiralling overspend meant the Department frequently faced “unpalatable options” about which services might need to be cut or temporarily suspended. Despite these efforts, additional funding still had to be sought from Tynwald.
“Health is a demand-led service. You don’t know what is coming through the door next.”
She was clear that Manx Care did not inherit a high-quality, fully integrated health system when it was established. Acknowledging the expectations placed upon the new organisation, she said she had never believed the transition would be smooth. “I expected it to be a bumpy ride,” she said, noting that it remains “obvious we haven’t got it right yet.”
Nonetheless, she emphasised that every member of Tynwald shares the goal of creating the best possible health service for the Isle of Man. To achieve that, she urged members to commit to working collaboratively, rather than focusing on division or blame.
Mrs Corlett also questioned whether the current operational structure between the Department and Manx Care is still fit for purpose. With several years now having passed since its introduction, she suggested that it is time to review how the two bodies interact and function together.
“The path to providing a quality care system that meets the needs of the residents while operating in a limited budget is a huge challenge. I would urge members not to look back with rose-tinted glasses.”
Vote
Tynwald approved the motion as amended by Health and Social Care Minister Claire Christian which removed the entirety of the wording contained within Lawrie Hooper's motion.
Her amendment reads:
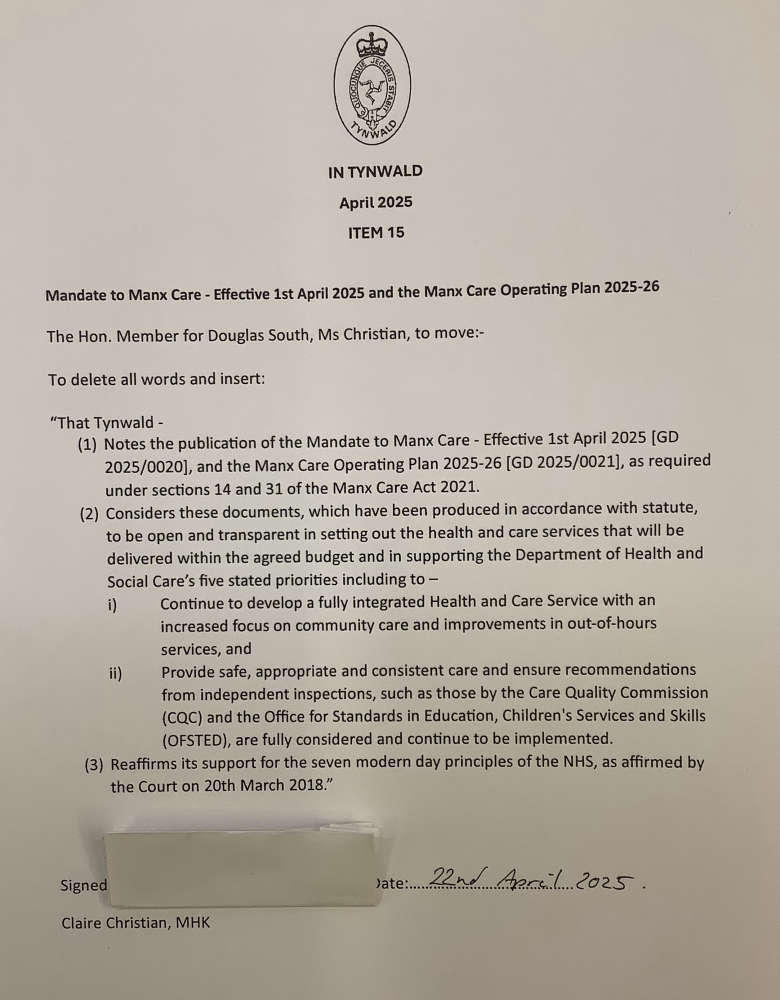
Ms Christian's amendment passed with 11 Members of the House of Keys in favour with eight against. Six Members of the Legislative Council voted in favour of the amendment, with two against.
As a result, Mr Hooper's attempt to challenge the Mandate and Operating Plan was defeated.


 Campaign to raise Isle of Man breastfeeding rates
Campaign to raise Isle of Man breastfeeding rates
 St John's sewage works 'operating within licence limits' despite concerns over discharge
St John's sewage works 'operating within licence limits' despite concerns over discharge
 Former MHK calls for climate change referendum
Former MHK calls for climate change referendum
 Access road constructed as Peel sewage works project progresses
Access road constructed as Peel sewage works project progresses
